Mending Broken Hearts
Using silk, scientists are working on ways to grow grafts for clogged coronary arteries
By Chris Berdik
A group of Tufts scientists has found a new weapon in the fight against heart disease, America’s number one killer. It’s not a special diet or a new pill. It’s silkworms.
Led by Michael Lovett, E09, a postdoctoral associate in Tufts’ Tissue Engineering Resource Center (TERC), the researchers are developing ultra-thin tubes made from silk that will serve as grafts for clogged coronary arteries. These grafts could replace the current standard for coronary bypass surgery, which involves harvesting a large vein from the lower leg—a procedure that is more invasive and not always suitable for patients with vascular disease. Silk has already been approved for other medical uses, ranging from sutures to artificial ligaments.

“The ultimate goal is that you won’t have a silk tube in there at all, because over time, your smooth muscle and endothelial cells will colonize the graft and recreate your artery,” says Michael Lovett, with one of the silk tubes. Photo: Alonso Nichols
As promising as this new application is, it wasn’t the original goal of the TERC researchers. Five years ago, when he was still a doctoral student in biomedical engineering, Lovett set out to give man-made tissue the ability to supply its dispersed cells with oxygen and nutrients through a network of blood vessels, a technique that would enable the researchers to grow thicker, stronger tissue. The lack of such a system has made it difficult to grow tissue more than a millimeter thick.
“That’s a far cry from the dream of engineering a pipeline of new organs,” says Lovett, who worked on the project with Chris Cannizzaro, a research assistant professor of biomedical engineering.
The pair decided to work with silk, one of the primary biomaterials used at TERC, a joint venture with Columbia University, and a focus of research by the center’s director, David Kaplan, professor and chair of biomedical engineering.
Their first challenge was to form tubes from the viscous solution made in the lab by boiling down silkworm cocoons. They tried dipping a stainless-steel wire into the solution and then removing the wire later. Next, they tried using a spinning wire and then shaving the tube with a blade. Neither method worked perfectly. Finally, they decided to follow the lead of silkworms and spiders, which spin their threads by expelling liquid silk through tiny holes, called spinnerets.
Successful at last, the researchers now squeeze silk solution through a small-gauge needle and wind the thread around a rotating and reciprocating spindle, creating a perfect tube of any diameter they choose in just minutes. The processing technique is called “gel spinning.”
But by the time they had perfected the gel spinning and built a machine to automate the process, Lovett’s research objectives had shifted.
As Lovett puts it, “We started thinking maybe these tubes themselves are interesting apart from just creating vascularized tissue,” or tissue that has its own blood supply. Along with collaborators at Columbia, with whom the Tufts TERC researchers meet once a month, Lovett started to focus on bypass grafts.
Engineering New Arteries
He spun tubes about one millimeter in diameter and tested their strength, flexibility and ability to handle flow. He seeded them with smooth muscle and vascular endothelial cells, observed how quickly and uniformly they grew throughout the tube and watched for any tendency to clot.
“The ultimate goal is that you won’t have a silk tube in there at all,” Lovett explains, “because over time, your smooth muscle and endothelial cells will colonize the graft and recreate your artery.”
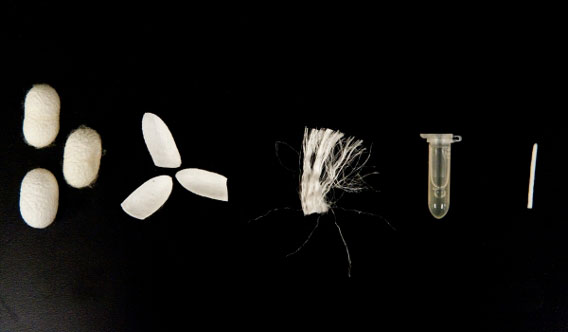
The silk used in the vascular grafting: from cocoon to silk fibers to melted silk protein and finally to narrow tubing. Photo: Alonso Nichols
In addition to the in vitro tests at Tufts, the silk tubes were implanted in the aortas of rats by George Eng, a doctoral and medical student at Columbia. So far, the tubes’ performance has been comparable to native tissue and better than the leading synthetic alternative, Teflon. In the rat experiments, a layer of cells envelops the entire tube within four weeks.
Lovett and his collaborators are now incorporating drugs into the tubes to better control the cell growth and further decrease the risk of clots. In addition, they want to ensure that the silk tube degrades at a rate that matches the re-growth of native tissue.
“If it goes away too quickly, the cells lose their support,” says Gordana Vunjak-Novakovic, a biomedical engineering professor at Columbia and that university’s principal TERC researcher. “If it goes away too slowly, then the material gets in the way of cell growth.”
The next step will be to try out the grafts in a larger animal, such as a pig or a sheep, and eventually move on to human clinical trials. The pace at which things progress to clinical care “all depends on resources,” says Kaplan. “If you found me somebody with a few million dollars to invest in this tomorrow, I’d say they’d be ready within a few years.”
In the meantime, researchers from other universities have contacted Lovett with ideas about using the tubes in other medical applications, including nerve guides and bladder augmentation, a common surgery in children with birth defects. Plus, there’s still the original focus of the research—providing the circulatory system the support needed to grow larger, more complicated tissues.
“If these tubes continue to work as we expect them to work, it would be big,” says Vunjak-Novakovic. As Lovett says, “You never know where research is going to take you.”
Chris Berdik is a freelance writer based in Boston.


