Potential Tumor Stopper
Gene is found that regulates cancer stem cells in a type of aggressive brain cancer
Tufts researchers have found a gene that regulates cancer stem cells in brain cancer, which could perhaps later become a target for doctors fighting a particularly malignant and aggressive type of brain tumor, the same type that Senator Edward Kennedy suffered from.
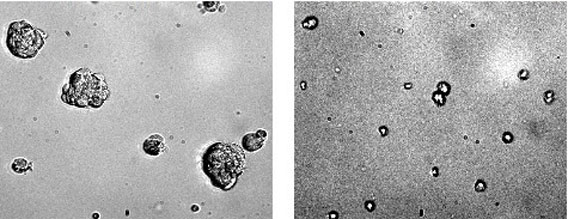
Glioblastoma stem cells in normal state on the left; on the right are the same cells with STAT3 inhibitor.
Cancer stem cells have many characteristics of stem cells and are thought to be the cells that drive tumor formation. The researchers report that the gene, called STAT3, could become a target for cancer therapy, specifically in Glioblastoma multiforme (GBM), a type of malignant and aggressive brain tumor. Patients with Glioblastoma multiforme typically survive 12 to 14 months with treatment. Treatment options include radiation, chemotherapy and surgery.
“When STAT3 is inhibited, cancer stem cells in glioblastomas lose their stem-cell characteristics permanently, suggesting that STAT3 regulates growth and self-renewal of stem cells within glioblastomas,” says senior author Brent Cochran, a professor at the School of Medicine and a member of the cellular and molecular physiology program faculty at the Sackler School of Biomedical Sciences. “Strikingly, a single, acute treatment with STAT3 inhibitors was effective, implying that a STAT3 inhibitor could stop tumor formation.”
STAT3 has been shown to be activated in a number of human tumors, Cochran says. But this study is one of the first to show that STAT3 regulates cancer stem cells. “It is one of the few genes linked to the propagation of cancer stem cells, and it appears to regulate processes involved in the six hallmarks of cancer: growth, metastasis, angiogenesis, evasion of apoptosis, tissue invasion, and cell immortalization,” he adds.
The researchers used cancer stem cells isolated from surgically removed samples of glioblastoma tumors. Cell cultures were treated with two chemically distinct small-molecule inhibitors of STAT3. After several days of treatment, cell growth in the STAT3-inhibited cultures was minimal compared to growth in the control cultures.
Moreover, in the STAT-inhibited cultures, proteins that help maintain stem-cell characteristics were apparently turned off. This finding leads the researchers to believe that STAT3 has a distinct role to play in cancer stem cells, which may make it an especially good target for cancer therapy.
“Current cancer therapies that prolong life do not specifically target cancer stem cells, and these cells are often resistant to traditional radiation and chemotherapies,” says Julian Wu, associate chairman of neurosurgery and chief of the division of neurosurgical oncology at Tufts Medical Center and a professor at the School of Medicine. “STAT3 appears to govern the propagation of cancer stem cells in Glioblastoma multiforme. Targeted inhibition of STAT3 in GBM cancer stem cells gives us a new approach to treating this devastating brain cancer.” Wu is known for his expertise in gene therapy for brain tumors and the molecular genetics of primary and metastatic brain tumors.
“We are encouraged by the potential of STAT3 in our study,” said Cochran. “Research has already demonstrated that STAT3 and cancer go hand in hand, but, until this study, we did not know that STAT3 regulates cancer stem cells, which are extremely resistant to conventional therapy. Given these findings, I hope that our future research investigating the mechanisms involved in inhibiting STAT3 will contribute to more effective and less invasive cancer therapies.”
The findings were published in Stem Cells in August. First author Maureen Sherry is a graduate student in cellular and molecular physiology at the Sackler School and is a member of Cochran’s laboratory.


