Not a Dry Eye
Stem cells could be used to repair damaged salivary and tear-producing glands
By Jacqueline Mitchell
Think about the smell of freshly baked bread wafting from the oven. Chances are your mouth is already watering. Beyond the purely sensory, saliva plays a crucial role in our ability to chew, swallow and digest food. It also helps keep our teeth cavity-free. But damage to the salivary glands, as well as the tear-producing lacrimal glands, can lead to major health problems, including organ damage and a higher risk for developing lymphoma.
A healthy salivary gland, the goal of Driss Zoukhri’s research efforts. Photo: BSIP/Photo Researchers, Inc.
Whether these glands stop working due to injury, often from radiation therapy for certain cancers, or diseases such as HIV and diabetes, the resulting dry eyes and mouth can severely affect a person’s quality of life.
But what if these damaged glands could be repaired? That’s not so far-fetched, says Driss Zoukhri, an associate professor of general dentistry at Tufts, whose research team has already demonstrated that at least in mice, injured lacrimal glands can repair themselves, quite possibly through an influx of stem cells, which have the potential to grow into any type of cell in the body.
Now, with a two-year, $1 million National Institutes of Health grant funded under the American Recovery and Reinvestment Act, Zoukhri will investigate the cellular mechanisms underlying that repair process. The researchers want to figure out where those stem cells are coming from and what cellular signals recruit the cells to the damaged glands to begin the repair work. Those discoveries could produce better treatments for people with damaged tear and salivary glands.
Each year about 40,000 Americans are diagnosed with head and neck cancers, for which radiation therapy is the first line of treatment. And up to 88 percent of patients who undergo radiation for those cancers will experience reduced salivary flow for more than a year.
Another four million people in North America suffer from Sjögren’s syndrome, an autoimmune disease that attacks tear and salivary glands, leaving patients—90 percent of them are women over age 45—with chronically dry eyes and dry mouth. Sjögren’s is one of the most common autoimmune diseases, and there is no cure. Sjögren’s can occur by itself, but more often arises in conjunction with another autoimmune disease, such as multiple sclerosis, rheumatoid arthritis or lupus.
Reversing the Damage
Tears and saliva, says Zoukhri, are chemical cousins, both consisting of water, electrolytes and proteins. Saliva is a bit stickier than tears, and the enzymes it contains help us digest carbohydrates. But both fluids are so similar that surgeons are able to re-route the salivary ducts of patients whose lacrimal glands have been permanently damaged so that their salivary glands produce moisture and lubrication for both the eyes and mouth.
In Sjögren’s patients, their body’s own immune system—by mechanisms not completely understood—attacks the glands’ cells and causes a decrease in salivary or tear flow without actually destroying the glands.
“When you look at biopsies from the salivary glands of Sjögren’s patients, in a lot of cases, 50 percent or more of the tissue is still intact,” Zoukhri says. “The glands should only need about 10 percent of the tissue to produce adequate secretion,” he says, “so we don’t understand why the remaining portion of the gland isn’t working.”
That provided an opening for researchers like Zoukhri to devise a way to reverse the damage and get the tears and saliva flowing again.
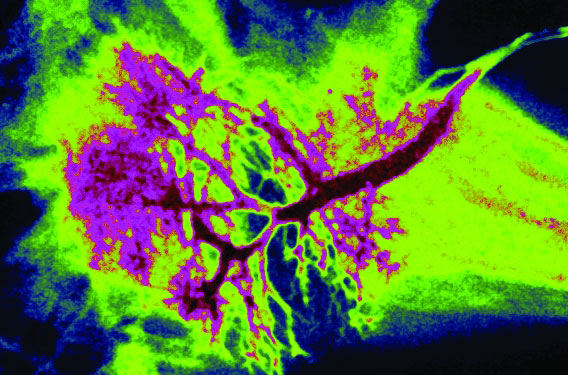
In an article published in the journal Investigative Ophthalmology & Visual Science in 2008, Zoukhri and his colleagues describe how they were able to induce, and then reverse, the symptoms of Sjögren’s syndrome in mouse lacrimal glands. They injected inflammatory cytokines—normally released by the body’s immune system to kill invading pathogens—into the mouse glands. After 24 hours, the cytokines attacked and effectively shut the glands down, mimicking the symptoms of Sjögren’s. But the effects were not permanent. “To our surprise, the lacrimal glands completely healed by days six and seven,” says Zoukhri.
The researchers found that in the glands they’d injected with cytokines, the lacrimal cells died by apoptosis—programmed cell death that occurs most often during embryonic development. They also found that the number of stem cells in the glands increased dramatically.
“We don’t know if the stem cells are recruited from elsewhere or are activated in the gland tissue,” says Zoukhri. He suspects that apoptosis triggers tissue repair by somehow sending the stem cells to the damaged glands, where they differentiate into new, healthy gland tissue.
His hypothesis is that a defect in the apoptotic process is what causes salivary and lacrimal glands to malfunction in people with Sjögren’s. (While the research published in 2008 was confined to the lacrimal gland, Zoukhri’s unpublished data show that the same principles apply to the salivary gland. “Diseases of one very often affect the other,” he says.)
With the new NIH funding, Zoukhri and his team will isolate the mouse stem cells, propagate them outside the body, and inject them into other animals with damaged glands. If the cells can restore glandular function, it could signify a breakthrough in treating people with Sjögren’s and other disorders of the tear and salivary glands.
It goes without saying that replacing, instead of repairing, diseased and injured tear and salivary glands would be the grail for treating disorders like Sjögren’s. To that end, Zoukhri is collaborating with Christophe Egles, an assistant professor at the dental school who works in the lab of Jonathan Garlick, director of the school’s Division of Cancer Biology and Tissue Engineering, as well as with David Kaplan, professor and chair of biomedical engineering at Tufts, to create artificial lacrimal and salivary glands.
“We’d ultimately grow artificial glands, implant them into animal models and see how they work,” says Zoukhri.
This article first appeared in the Spring 2010 issue of Tufts Dental Medicine magazine.
Jacqueline Mitchell can be reached at jacqueline.mitchell@tufts.edu.