How We Die
In his new book, a Tufts psychiatrist explains why end-of-life care is not murder
By Jacqueline Mitchell
When Massachusetts State Police knocked on Amy Gleason’s door in December of 2001 and told her they were investigating a death, her mind leapt first to her husband and then to her father. But slowly, as the investigators asked more about her work, Gleason realized the death was one that had occurred weeks before, in the renal unit at Baystate Medical Center in Springfield, Mass., where she was an experienced dialysis nurse.
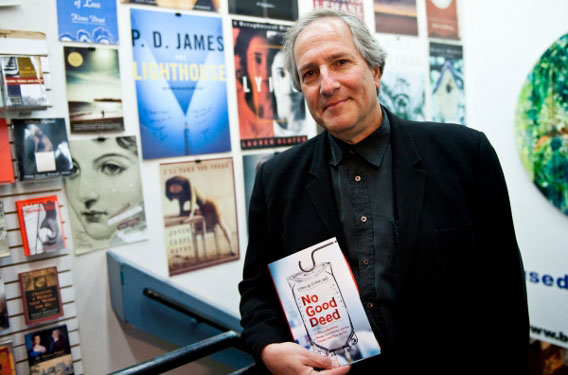
“Far too few patients are told what their prognoses really mean,” says Lewis M. Cohen. Photo: Alonso Nichols
She and fellow nurse Kim Hoy were being investigated for the murder of a severely ill patient, Rosie Doherty, a woman so sick with kidney failure, vascular disease, diabetes and emphysema that Hoy described her as “necrotic . . . basically, she was rotting.”
Though Doherty was alert periodically, she was never fully oriented or coherent. Because she was unable to speak for herself and make the decision to stop treatment, her family, physicians and nurses together agreed to move from curative medical treatment to palliative, or end-of-life, care. This meant Doherty’s caretakers would no longer treat her manifold illnesses or subject her to dialysis treatments, but instead make her as comfortable as possible during her few remaining days.
While many health-care providers consider withdrawing treatment and letting a patient die a legitimate option, some consider it murder. That’s why a nursing assistant who witnessed Gleason and Hoy providing palliative care to Doherty took her concerns to the district attorney. The ordeal was a traumatic one for all involved, from the whistleblower to the accused nurses to the patient’s family, who learned the day of Doherty’s funeral that the police wanted to “impound the body.”
Inside and outside the medical profession people still view palliative care as “an unseemly sprint towards death,” says Lewis M. Cohen, a professor of psychiatry at the School of Medicine and a clinician-researcher based at Baystate. An expert in palliative care, Cohen won a Guggenheim Fellowship to work on his new book, No Good Deed: A Story of Medicine, Murder Accusations, and the Debate Over How We Die (Harper, 2010). In it, Cohen uses the murder investigation at his own hospital to examine the controversy surrounding end-of-life care.
Tufts Journal: Why did you write No Good Deed? What do you hope readers will come away with?
Lewis M. Cohen: This book is not about physician-assisted suicide; it’s not about psychopathic nurses who really are serial killers; it’s not about medical catastrophes like what happened after Hurricane Katrina. This is about well-meaning doctors and nurses who believe they are providing medically appropriate end-of-life care and are then shocked to find themselves accused of murder. It’s a completely unexpected event when it happens. Physicians and nurses are accustomed to a certain amount of controversy, and those conflicts can sometimes turn into malpractice. But the idea of it actually turning into criminal accusation and people having to defend themselves are extraordinary occurrences.
That’s the main story, about the case that happened at Baystate, which I learned about a couple years after the fact. But the book also discusses other nurses and physicians around the country who are in similar circumstances, who face public humiliation, loss of jobs, bankruptcy, criminal trials and, in some cases, literally being sent to the penitentiary.
Palliative care has gained widespread acceptance among the medical professions over the last 20 or 30 years, but do health-care workers appreciate the controversies surrounding it?
I didn’t myself, until two things happened. One was the Terri Schiavo case that was beamed into our living rooms. And suddenly we saw images of people coming to protest at the hospice and began to hear the interviews with the family and their supporters. The other was this case in my own hospital, with a very actively involved DA.
The only sense I could make of it was that there is this underlying conflict that has grown up between organized medicine—especially those who maintain the philosophy of palliative care—and this other philosophy, which holds that many of the tenets of palliative care are totally unacceptable, immoral and may or may not be illegal.
Some of the religious-based objections to withholding or withdrawing life support come from the idea that to do so is to interfere with God’s will. How do people and institutions determine where the line lies between medical care and God’s will?
I personally found making sense of religious views on this topic to be very difficult and in some ways over my head. What I found is that different theologies hold different beliefs, and even the same church, like the Catholic Church, may hold disparate beliefs.
There are nuances in how they think about things, and there have been changes in how they think about things. To stay with the Catholic Church, for example, that’s an institution which up until probably the last 10 years has been extraordinarily understanding of what we do in hospitals. The Church has been very comfortable with medicine offering not only extraordinary measures, but also reaching the point where either the physician or the patient, or hopefully everyone involved, feels that extraordinary measures no longer make sense and it’s time to either withdraw or withhold them. For maybe 450 years the Church has been in line with that stance.
Over the last 10 years or so, one sees a more conservative element, which is closer in line with the vitalist philosophy. Vitalists are more uncomfortable with withdrawing certain life supports such as feeding tubes and, in general, are more uncomfortable with any measures that take place in hospitals that might shorten people’s lives.
Does some of the opposition to palliative care seem like it’s based on the lay person’s unfamiliarity with modern medicine and its limitations?
I don’t think people are provided with enough of the information that would allow them to make decisions that are consistent with the beliefs of the patient or the family. Far too few patients are told what their prognoses really mean. Speaking from my position as a physician, we’ve been hesitant to tell patients what else the future holds for them besides life and death.
For example, it’s one thing to give a patient a diagnosis that he or she doesn’t have long to live. But I think we also ought to be telling people who, for example, are facing a particular surgery in which 75 percent of people undergoing this surgery will end up in nursing homes and will likely never go home again. Or there’s a 50 percent chance you’ll have to remain on a ventilator. Those conversations are still fairly uncommon, and I think that’s one barrier to people making well-reasoned decisions.
Some worry about people making end-of-life decisions when they are emotionally distraught after receiving bad news. How can physicians address this?
The standard answer is that, minimally, every one of us should be appointing a health-care proxy, someone who can speak up for us when we can’t speak up for ourselves. That’s the quick answer, but the more honest answer is, I don’t know if people in their 20s and 30s can honestly grapple with these situations, these possibilities. It’s a developmental leap. It can be easier to think about if you’ve had a parent who has died. This book is coming out on my 60th birthday. It’s easier for someone my age to think about these matters.
Speaking of people in their 20s and 30s, do you believe today’s medical students are adequately schooled in these matters?
Palliative medicine is a brand new specialty that was granted specialty status in the last couple of years. We have a new generation of medical students waking up to the idea that palliative medicine is actually a full-fledged specialty, and it can become their specialty, too, if they so choose.
Additionally, bioethics has become more important to medicine as medicine has become more successful and more complicated. Today’s medical students have the opportunity to train under bioethicists and to think about these matters. When I have Tufts third-year medical students rotate through my workplace, they often sit in on cases that bring up end-of-life matters, so they’re getting an opportunity to talk and think about it, too.
You found that the power differential between doctors and nurses, on one hand, and between nurses and nurses’ assistants caused some of the misunderstandings and miscommunications regarding end-of-life scenarios. How so?
I didn’t really appreciate it until I started to talk to the nurses for this book. I’m someone who’s considered an expert in end-of-life matters, and have written extensively and lectured before large groups about it. Yet I had this dawning awareness that I’ve been at the bedside of very, very few people when they died. Any of the renal nurses or oncology nurses I meet probably has vastly greater experience with death than I do. That was kind of the lightbulb going on in many ways. And then this particular case turned up the wattage of the lightbulb. I’ve come to understand that it’s the nursing assistant—we call them technical associates or TAs at Baystate—who are, in fact, even more likely to be present at the time that people die, because they are the ones who spend so much time at the bedside.
If we accept this, what can we do differently? I think we as physicians can extend ourselves to the TAs, or even to the guy who goes into the room pushing a broom, and provide them with some educational opportunities to hear about what medicine thinks about death. I would also give them a chance to speak their minds. Then, when they encounter something [like this case], they won’t feel like they have to go to a disciplinary body like the district attorney’s office to lodge a complaint, but rather they’ll feel like they are working in an institution that wants to hear what they have to say.
Jacqueline Mitchell can be reached at jacqueline.mitchell@tufts.edu.


