Breathing Easier
Research at the Cummings School offers hope for innovative treatments for emphysema
By Catherine O’Neill Grace
Imagine having to think about every breath you take. Imagine gasping after you walk across a room. Imagine breathing in, and then being unable to expel that breath without effort. That’s how people with emphysema live. The condition—a type of chronic obstructive pulmonary disease—involves progressive and irreversible damage to the air sacs in the lungs and affects more than 3 million Americans, killing 120,000 every year.
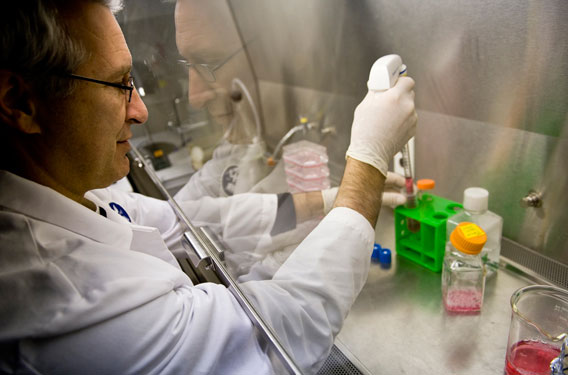
“We are focused on rebuilding the lung,” says Andrew Hoffman. Photo: Alonso Nichols
The physical effect of emphysema on the lungs is like “cutting parts of a cobweb or a net. The lung just starts to unravel,” says Andrew M. Hoffman, a professor of large animal medicine at the Cummings School who researches treatments for lung disease in animals and humans.
It is well known that cigarette smoking is the major cause of emphysema. What’s not known is how the condition spreads in the lung, and whether that process can be halted or reversed.
But hope may be on the horizon, thanks in part to research Hoffman is conducting with support from the National Institutes of Health. He and his colleagues have devised a method to mitigate the symptoms of the disease, using a special kind of epoxy to reduce lung volume, which allows the remaining lung to take in and expel air more efficiently. Now they’re trying to develop ways to rebuild lungs, cell by cell.
As a large animal veterinarian, Hoffman has specialized in diagnosing and treating equine lung disease, which develops from chronic exposure to dusty barns and racetracks and is similar to human chronic obstructive pulmonary disease (COPD). To study emphysema—a type of COPD—he has focused on sheep, since their lung size and anatomy closely resemble those of human lungs. He is collaborating with Edward Ingenito, an assistant professor of medicine at Harvard Medical School and an associate physician at Brigham and Women’s Hospital in Boston.
“We developed methods to evaluate the safety and outcome of treatments intended for humans in the sheep models, and a long-term collaboration between human pulmonologists and veterinary physiologists was born,” says Hoffman.
Ingenito and Hoffman found a non-invasive way to improve lung function in animals and humans, which is now in the final phases of clinical trials. The so-called bronchoscopic lung volume reduction technology uses special glues to reduce the size of the emphysema-affected lung, allowing the remaining lung to work more efficiently. The treatment could mark an important advance in emphysema therapy. Ingenito is the founder of Aeris Therapeutics, a medical company with offices in Woburn, Mass., and on the Cummings School campus that holds the patent for the volume reduction technology.
Additional important advances could follow. “Using the biocompatible glue to close off the emphysema-damaged lung allows patients significant relief, but the disease will continue to progress,” Hoffman says. “Part of the reason for that is that patients have already lost a lot of their critical progenitor and stem cells in the lungs—and there’s not much known about stem cells in the lung yet.” He points out, however, that “the lessons that we learned in developing volume reduction have better prepared us for developing stem cell therapy [for emphysema]. We have learned to take things from animals all the way up to humans.”
Using Stem Cells
Stem cells and progenitor cells are microscopic building blocks of the body. Progenitor cells are specialized in their functions, destined to become only one type of cell when they mature, such as a muscle cell or the particular type of cell that forms alveoli, or air sacs, in the lung. Stem cells, by contrast, have the potential to develop into a variety of cell types and have the ability to replenish damaged cells in many different organs. When a stem cell divides, each new cell created has the potential to remain a stem cell or to become another type of cell, such a red blood cell or a brain cell. Stem cells can replicate indefinitely, while progenitor cells can divide a limited number of times.
“We know that stem cells and progenitor cells are necessary to maintain a healthy cell population in the lung,” Hoffman says. If lung cells get injured, they can be replenished. “It’s just like your skin: When a few cells come off, new cells come up. The lung also has that capacity to replace certain cells with progenitor cells. With emphysema, those healing cells are targeted and damaged. If you lose your progenitors, you can’t respond to injury any longer.”
Hoffman and his colleagues have worked with lung cells from mice and sheep and with healthy human lung cells harvested through biopsies. Their goal has been to develop ways to grow new progenitor cells from existing healthy cells. Because such cells would be identical to the host lung cells, the diseased lung would be less likely to reject them.
“We are focused on rebuilding the lung,” says Hoffman. “We want the cells to actually build new air sacs.” The idea is that the new progenitor cells would attract “the other two main types of cells—those on the blood side of the lung’s structure and those on the air side.” This could allow fine blood vessels to “run through and pick up oxygen,” lessening the breathing problems patients with emphysema experience.
Hoffman and his colleagues have been able to demonstrate that the lab-grown progenitor cells produce everything they hoped they would. “They produce elastin [which allows the lung cells to expand and contract] and growth factors and are capable of assembling the scaffolding that other cells can attach to,” he says. “We have demonstrated that they have the potential to replace damaged cells in the emphysema lung.”
They have also isolated progenitor cells, grown them and put them in mice and sheep with encouraging results. “We have done two different pre-clinical trials in sheep, and both showed that the cells improved blood flow and increased tissue mass in the emphysema lung,” says Hoffman. He hopes that at the conclusion of his study, in about five years, the lung-rebuilding technique can be tested safely in human emphysema patients. The technology that is being developed to treat emphysema could also potentially be applied to a variety of lung disorders that, while less common, are equally serious.
Catherine O’Neill Grace is the editor of Tufts Veterinary Medicine magazine. She can be reached at catherine.grace@tufts.edu.


